Sjogren Syndrome
- related: Rheumatology
- tags: #rheumatology
Epidemiology and Pathophysiology
Sjögren syndrome is an autoimmune exocrinopathy affecting salivary and lacrimal glands. It is more prevalent in women and White persons and commonly presents in the fourth and fifth decades. Primary Sjögren syndrome occurs in isolation; secondary Sjögren syndrome occurs in the setting of other rheumatologic diseases, most commonly rheumatoid arthritis and systemic lupus erythematosus. Whereas the prevalence of primary Sjögren syndrome ranges from 0.5 to 5 patients per thousand, secondary Sjögren syndrome is common (10%-30%) among populations with predisposing rheumatologic conditions. Sjögren syndrome etiology remains unclear, although genetic associations include several HLA subtypes.
Clinical Manifestations
The most common presentation of Sjögren syndrome is sicca, consisting of dryness of the eyes (keratoconjunctivitis sicca) and mouth (xerostomia). Patients report gritty eyes or a foreign body sensation. Oral dryness can cause caries and difficulty eating unmoistened food. Symmetric parotid and lacrimal swelling is common, as is skin and vaginal dryness.
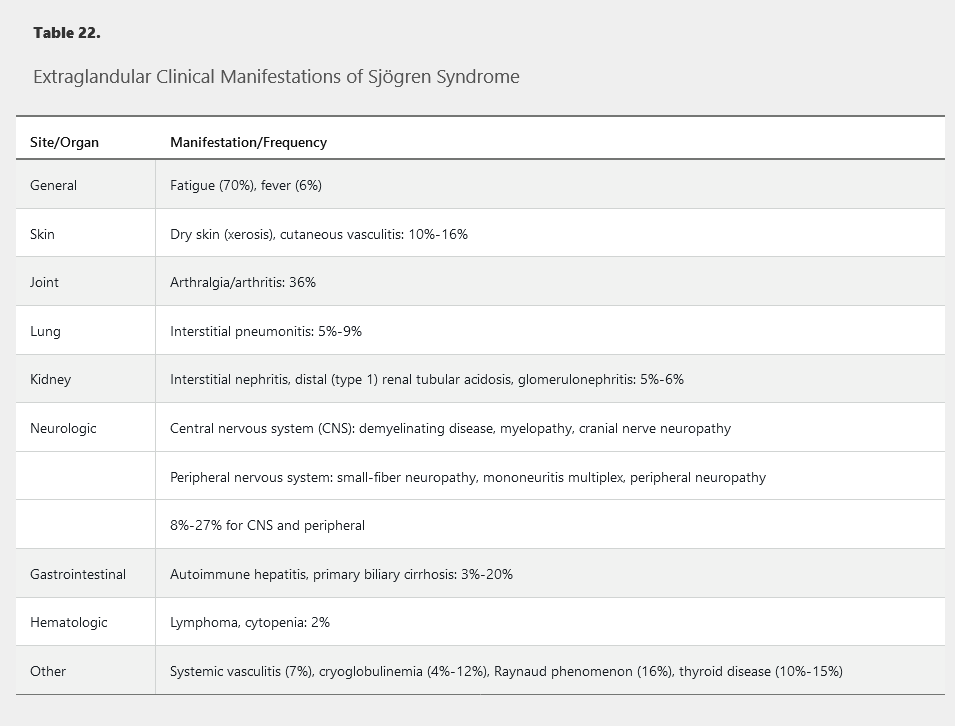
Extraglandular manifestations may also occur (Table 22). Arthralgia and arthritis are common; the joint distribution and presentation resemble rheumatoid arthritis but without bone erosions (Jaccoud arthropathy). Patients with Sjögren syndrome are at increased risk for non-Hodgkin lymphoma, presumably related to chronic lymphocyte activation.
The most common renal manifestation of SS is chronic interstitial nephritis. Patients with this condition usually have mild renal insufficiency, a fairly benign urinalysis, and renal tubular abnormalities such as distal renal tubular acidosis (leading to metabolic acidosis with hypokalemia) and nephrogenic diabetes insipidus (leading to low urine osmolality, frequent urination, and excessive thirst).
Diagnosis
A diagnosis of Sjögren syndrome is typically triggered by a complaint of sicca and requires objective confirmation of exocrinopathy along with demonstration of autoimmunity (Table 23). Dry eyes can be assessed using the Schirmer test, in which a strip of filter paper is placed under the lower eyelid and wetting is measured; less than 5 mm in 5 minutes indicates dryness. More formally, dryness and corneal damage are ascertained by slit-lamp examination by an ophthalmologist using fluorescein and lissamine green dyes. Dry mouth is assessed by direct examination, with dental caries and a lack of saliva suggesting the diagnosis. Measurement of salivary flow (sialography) is easily done, and salivary scintigraphy may also be considered. Salivary gland imaging with MRI or ultrasonography may assist in identifying characteristic abnormalities and provide additional support for the diagnosis.
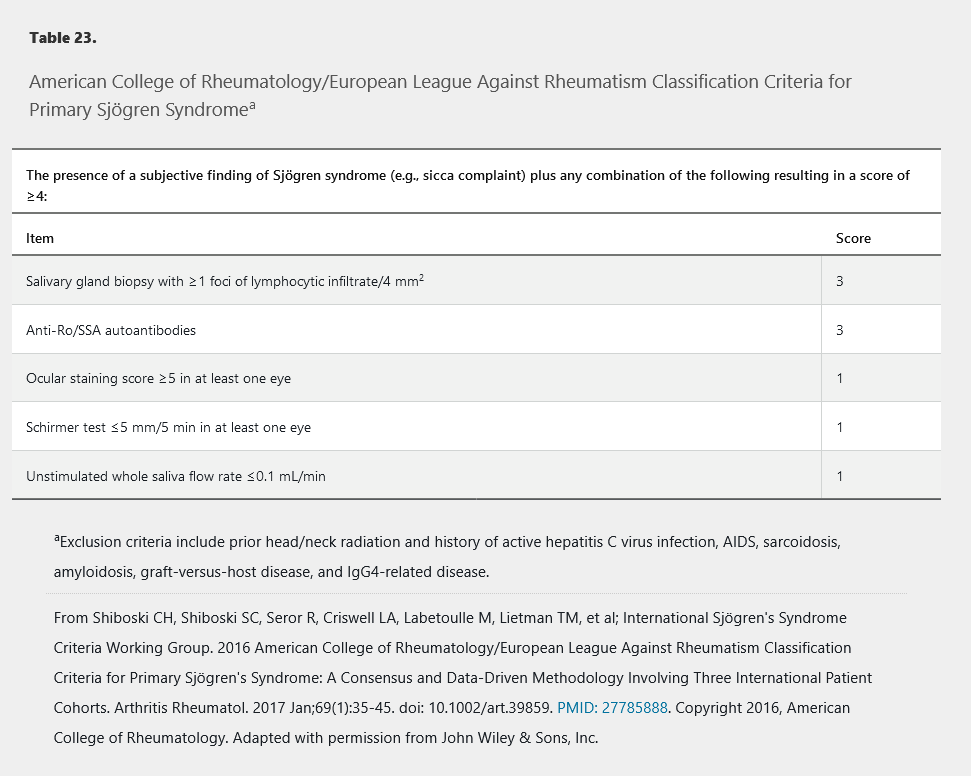
Multiple autoantibodies may be present. Antinuclear antibodies and/or rheumatoid factor are often present at high titers; their coexpression is more suggestive of Sjögren syndrome than if only one is positive. The presence of anti-Ro/SSA autoantibodies is specific in the setting of primary Sjögren syndrome; their presence is less specific for secondary Sjögren syndrome because these antibodies are also common in systemic lupus erythematosus. The presence of anti-La/SSB autoantibodies is also characteristic of Sjögren syndrome, although these are not currently included in formal disease classification criteria. When initial evaluation is uninformative, a lip (minor salivary gland) biopsy should be considered. Characteristic histologic features include aggregate foci (>50 cells/aggregate) of CD4 T cells, B cells, and plasma cells surrounding secretory ducts.
The differential diagnosis of Sjögren syndrome typically relates to the presence of sicca and/or parotid and lacrimal enlargement. Sarcoidosis, IgG4-related disease, granulomatosis with polyangiitis, lymphoma, and viruses such as mumps, hepatitis C, and HIV may be associated with similar findings. Ocular and oral dryness may also occur with aging or in response to drugs such as anticholinergics.
Management
Management of sicca is centered on preservation of moisture and relief of symptoms. Eyes are treated with artificial tears. Patients with refractory or severe ocular dryness should be managed by an ophthalmologist and may be treated with topical cyclosporine. The use of glasses with side panels to prevent surface drying may be helpful, as may be plugging of the lacrimal ducts to promote tear retention. Before initiation of treatment for oral dryness, assessment of salivary gland function is recommended. For oral dryness, meticulous dental care is essential. Sugar-free candies and chewing gum can stimulate saliva flow. Regular intake or rinsing with small sips of water is also recommended. Pharmacologic therapies for moderate dysfunction include the muscarinic agonists pilocarpine and cevimeline, although these may not be well tolerated and are contraindicated in narrow-angle glaucoma. Artificial saliva may be used for severe dysfunction, but its effects may be too transient to be useful. Vaginal symptoms may be treated with topical lubricants or estrogen.
Patients with extraglandular involvement are treated with immunosuppression. For active systemic involvement, glucocorticoids may be considered a first-line option, but only the minimum dose and length of time necessary to control active systemic disease are recommended. Immunosuppressive agents and biologics should be used as second- and third-line agents in patients with severe disease or as glucocorticoid-sparing agents. Options include hydroxychloroquine and methotrexate for arthritis, and cyclophosphamide and rituximab for severe or systemic central nervous system disease. Some of these agents may have benefit for sicca as well.
Prognosis
The prognosis for primary Sjögren syndrome is favorable, with no overall increase in mortality. Management of sicca reduces the risk of corneal damage or loss of teeth. In rare instances, end-organ involvement can be life-threatening. Secondary Sjögren syndrome may be associated with significant morbidity from the primary condition. An increased risk of B-cell lymphoma is present in both forms of the syndrome.